Create Jira Ticket
This idea cannot be sent to Jira.
Pandemic Maps
HHS and CDC currently provide pandemic maps that are focused on state level reporting. This introduces problems for pandemic response coordination, in so far as these state level maps tend to group urban and rural interests together.
In general, HHS and CDC data reporting is in need of higher resolution and higher fidelity data visualizations, which can provide granulized policy guidance. Collecting data at the county or health service area (HSA) level could solve this problem, allowing data to be displayed and visualized at a more granular level.
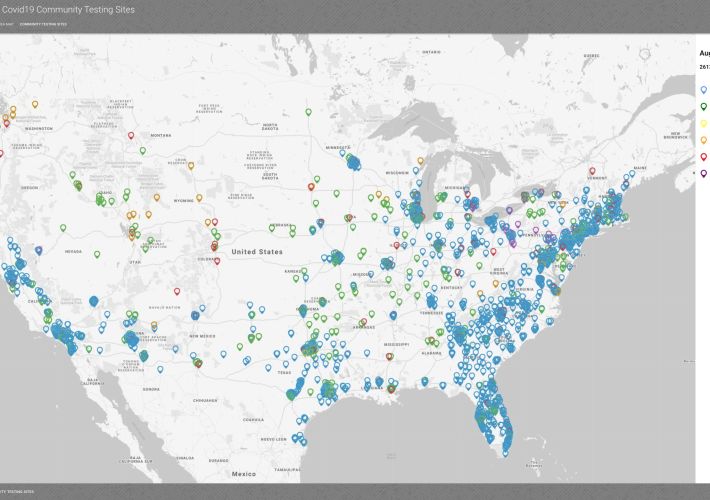
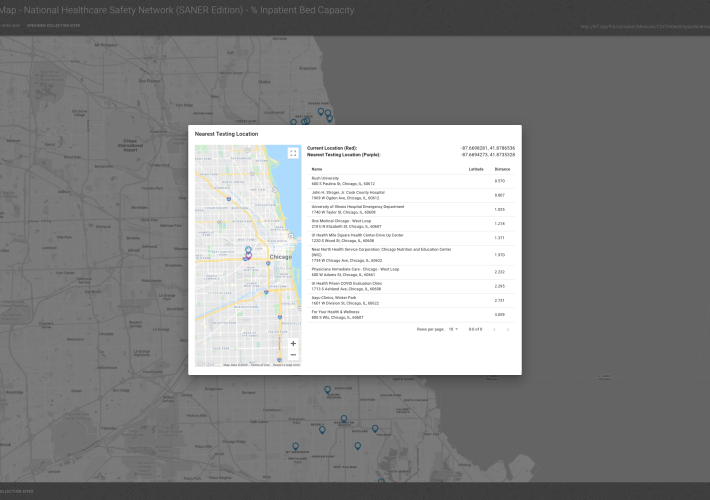
Symptomatic has been working to increase the resolution and fidelity of pandemic GIS reporting, and bringing pandemic mapping down to the county and HSA level data. We have been doing this by working with HL7 International, MITRE, and the CDC in developing an implementation of the SANER (Situational Awareness for Novel Epidemic Response) specification, which we then geocode and feed into Google Maps.
Our GIS/mapping solutions incorporate both choropleth maps and heatmaps, mobile device geolocation, hospital capacity metrics, community testing locations, nearest test site searching, municipal and national level health data reporting, and numerous other features.
Additionally, our GIS mapping solution runs on both web and mobile devices, and we're currently preparing to deploy to the Apple App Store, as well as the Epic App Orchard and Cerner Code Gallery.
Any design suggestions or feedback would be much appreciated. We're currently looking for pilot sponsors to assist in the rollout via the EHR app stores. If you have any geomapping needs, please reach out!










Trying to understand how your approach would address the following (In general) 1. How to collect AOEs, from ordering provider/patient/specimen collector 2. Integrate into app/LIS or other information source for patient to be married to results of IVD test device/system (either lab performed or patient performed at home like pregnancy test) 3. All transmitted to public health (ELR) 4. All transmitted to HHS (may be met by 3).
With the geomapping features, would data from several health jurisdictions be able to be measured/mapped the same way for better understanding of the data? For example, people work in Chicagoland and live in IN, MI, WI, and IL. IDPH data is mapped at zipcode level, while WI data is mapped at census tract level. Folks living in one state and working/shopping in another may not be measured the same way in each state to monitor border area clusters/movement/cases. Perhaps some public health folks can chime in, if it might be helpful to see. Similarly with IN/IL border, whether urban/surburban or more rural the further South they travel.
https://abc7chicago.com/mers-munster-communit...al-virus/44979/ The first MERS case arrived at O'hare and traveled to Munster, IN in 2014.
With many community "spreader" events would be interesting to see where individuals have traveled (cell data or other indicator), how many were clustered in close proximity (i.e. party, wedding, other gathering) and where they went or returned to (across the county, state, nation). The FL Spring break models were interesting as folks returned, a number brought the virus with them.